Raymond L. Woosley, MD, PhD, Raymond David Woosley, MPH and C. William Heise, MD
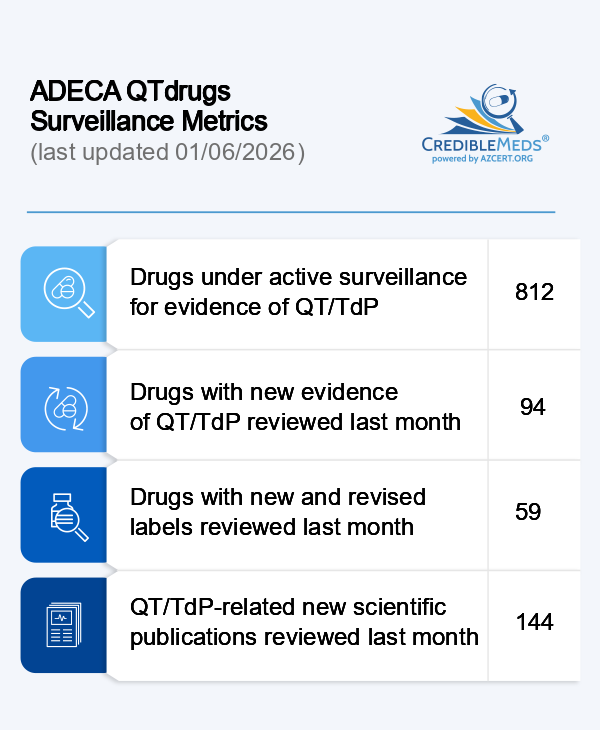
Prolongation of the QT interval is a well-established risk factor that predicts increased mortality from sudden cardiac death.1 Identification of patients with the highest risk of QT prolongation and associated adverse outcomes has been facilitated by the use of QT risk scores that have greater predictive accuracy than the QT interval alone. These scores take into consideration the many clinical conditions and medications that can contribute to QT prolongation.2,3 Most of these risk scores have used AZCERT’s QTdrugs List, a web-based list of drugs that prolong the QT interval and are known to cause torsades de pointes (TdP).
In 2015, AZCERT established a collaboration* with the University of Arizona College of Medicine-Phoenix, Banner Health, and researchers from the University of Utah and Purdue University with the goal of developing and evaluating a Torsades Advisory as a clinical decision support tool operating in 29 clinics and hospitals in the Banner Health system. This has since been expanded to include the entire network across the western US.
The Torsades Advisory works within Banner’s Cerner electronic medical record and calculates a QT risk score for each patient prescribed one of the 57 medications that AZCERT has designated as having Known Risk of TdP. When a patient’s QT risk score crosses a critical threshold, the prescribing physician receives a Torsades Advisory informing them of the patient’s increased risk of Torsades, the factors that contribute to the score and options for how to mitigate that risk. This clinical decision support tool was designed to focus on those patients at highest risk and to avoid actions that would result in “alert fatigue”.
Banner Health’s Torsades Advisory has been evaluated by AZCERT and its collaborators and the results published in three scientific articles which found that the Torsades Advisory 1) resulted in risk-mitigating actions being taken by 1/3 of prescribers within one hour,4 2) provided information that was considered to be valuable by 79% of prescribers surveyed5 and 3) identified a patient population that had an 11.5 fold greater mortality rate, generally proportional to their QT risk score.6
Based on these results, AZCERT has created a web-based QT/TdP decision support program for open use at MedSafetyScan.org. MedSafetyScan® is being used by thousands of clinicians around the world and has been scientifically evaluated and found to be clinically useful in a psychiatric population.7
*Partial funding provided by the Flinn Foundation, Phoenix, AZ, the Arizona Biomedical Research Commission (ABRC), Food and Drug Administration and the federal Agency for Healthcare Research and Quality (AHRQ). Reference List
- Schwartz PJ, Wolf S. QT interval prolongation as predictor of sudden death in patients with myocardial infarction. Circulation 1978;57:1074-7.
- Tomaselli Muensterman E, Tisdale JE. Predictive Analytics for Identification of Patients at Risk for QT Interval Prolongation: A Systematic Review. Pharmacotherapy 2018;38:813-21.
- Stettner S, Adie S, Hanigan S, Thomas M, Pogue K, Zimmerman C. Effect of Replacing Vendor QTc Alerts with a Custom QTc Risk Alert in Inpatients. Applied clinical informatics 2022;13:19-29.
- Gallo T, Heise CW, Woosley RL, et al. Clinician Responses to a Clinical Decision Support Advisory for High Risk of Torsades de Pointes. J Am Heart Assoc 2022;11:e024338.
- Gallo T, Heise CW, Woosley RL, et al. Clinician Satisfaction With Advanced Clinical Decision Support to Reduce the Risk of Torsades de Pointes. J Patient Saf 2022;18:e1010-e3.
- Tan MS, Heise CW, Gallo T, et al. Relationship between a risk score for QT interval prolongation and mortality across rural and urban inpatient facilities. J Electrocardiol 2023;77:4-9.
- Demler TL, O'Donnell C. Navigating the pharmacologic complexities of QTc prolongation: assessing the cumulative burden in individuals with serious mental illness. Int Clin Psychopharmacol 2023.